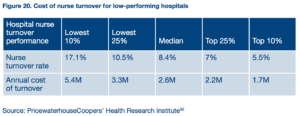
As we recently wrote about, the problem of nurse burnout and the challenge of figuring out how to engage, satisfy, and retain nurses is one that facilities who care about their bottom line can no longer afford to ignore. Nurse turnover is expensive.
And with the development of quality initiatives like accountable care models and episode-based payment, hospital and health system revenue is increasingly tied to measures related to patient satisfaction, health outcomes, and compliance with evidence-based standards of care. For example, one-third of Medicare payments to hospitals are now based on quality or value, including a growing portion of Medicare payments based on patient satisfaction scores from HCAHPS.
As a result, hospitals have focused heavily on reducing waste and improving standards of care. But these efforts add to the already overwhelming workload of clinical staff. At the same time, hospitals are trying to do more with fewer resources, often resulting in staffing shortages.
Nowhere is this push and pull situation—the need to improve care quality and patient satisfaction on one hand and reduce costs on the other—more acute than in nursing. No care providers have a bigger impact on patients’ experience of or satisfaction with their care than nurses, so keeping nurses engaged and satisfied is critical. And as the largest group of healthcare providers, nursing staff often represent the biggest labor cost for facilities. This can result in tension between the need to ensure appropriate staffing levels for safe, effective patient care and nurse sanity, and the need for facilities to remain financially viable.
and pull situation—the need to improve care quality and patient satisfaction on one hand and reduce costs on the other—more acute than in nursing. No care providers have a bigger impact on patients’ experience of or satisfaction with their care than nurses, so keeping nurses engaged and satisfied is critical. And as the largest group of healthcare providers, nursing staff often represent the biggest labor cost for facilities. This can result in tension between the need to ensure appropriate staffing levels for safe, effective patient care and nurse sanity, and the need for facilities to remain financially viable.
Many facilities’ leadership teams are asking nurses to do more with less as healthcare delivery becomes more complex: Balance more time spent documenting care processes through EMRs and other new mandates with the time, mental focus, and emotional energy needed to improve care coordination and patient satisfaction. It’s a lot for anyone—even someone as competent and compassionate as a nurse—to handle.
Nurse managers have complex jobs, and the role differs depending on department size, type, and other factors. But boiled down to the essentials, the three priorities that place these experienced nurses at the center of this tension are:
- Oversee patient care, ensuring quality, safety, and effectiveness.
- Manage department nursing staff, including recruitment, coaching, counseling, and mentorship.
- Set and stay within department budget, including labor, supplies, and other costs.
One issue central to staff nurse and nurse manager job satisfaction, care quality, patient satisfaction, and labor costs is staffing and scheduling. Many studies have shown nurse managers spend an inordinate amount of their time on this task, and that generally, they aren’t able to spend enough time on what they feel is most important. For nurses, reports show working conditions and schedules are the greatest influence on overall job satisfaction, with salary taking third place. And mandated nurse-to-patient ratios are a hot-button and divisive issue.
There are several ways that proactive nurse managers can begin to foster mutually beneficial staffing and scheduling to create a win-win situation for everyone (nurses, managers, facilities, patients), and technology like Nursegrid Manager can help.
- Simplify nurse-initiated schedule changes. Technology can make it easy for nurses to find colleagues available for swaps and giveaways, initiate those changes themselves from their smartphones, and provide managers with an easy way to review and approve or deny. Managers save a lot of time and nurses get quick responses without having to follow a paper trail at work.
- Communicate with nurses effectively: Communication is often cited as a priority for departments working to improve nurse engagement. Making communication more targeted—sending open shift opportunities only to nurses who’ve indicated they’re available to work, for example—can increase response rate and help nurses feel less overwhelmed. And using technology like smartphone push notifications means managers and schedulers can spend less time on phone trees.
- Intelligently adjust staffing levels as patient census and acuity fluctuate: Technology can surface the information you need around nurse preferences and availability when you need it and make it easier to do what’s right for patients and nurses while avoiding costly overtime and nonproductive time.
- Choose easy to use technology: Many nurses, particularly of older generations, are wary of technology that makes their working lives more complex, and with good reason. Easy to use and simple to implement technology is critical to get your staff working together across generations to adopt it—and tech clearly built just for nurses and nurse leaders helps too.
- Give nurses more ways to connect with one another: Studies have shown higher levels of teamwork within a unit increase job satisfaction. Technology can give nurses an easy way to engage with colleagues and managers. And though it might sound silly, seeing who they’re working with ahead of time is something our Nursegrid Mobile (a free mobile app for nurses) users love—and anyone who’s spent a long shift with an uncooperative colleague or a close friend knows why!
Whether you’re a seasoned nurse manager, brand new to the job, or thinking about making the transition, share any ideas you have in the comments below!
Get our latest white paper on nurse engagement and retention.
